2 Technology Place
Macquarie University NSW 2109
Restoring lymph flow by bypassing the damaged area
In lymphovenous anastomosis (LVA) surgery, the surgeon connects a lymph vessel in the affected limb to a nearby vein to bypass the damaged area and restore the flow of lymph fluid back to the venous system.
Lymphatic fluid surrounds the cells and tissues of the body and not only keeps the cells healthy, but also helps drain away waste products.
Lymph vessels transport lymphatic fluid from the limbs through the lymph nodes to larger lymphatic vessels which in turn join to large veins at the bottom of the neck.
When the lymphatic system is not working properly, the lymph fluid builds up and causes swelling, leading to the condition known as lymphoedema.
LVA gives the best results in patients with early-stage lymphoedema when the lymphatic channels are still working and healthy, and before irreversible damage – such as skin and tissue changes and fatty deposition – occurs.
In lymphovenous anastomosis (LVA) surgery, the surgeon connects a lymph vessel in the affected limb to a nearby vein to bypass the damaged area and restore the flow of lymph fluid back to the venous system.
Several connections are made, with the number depending on the condition of the lymph vessels. The connections are generally made before the damaged area and are performed using a small cut just below the surface of the skin. The surgery is performed under general anaesthetic.
A vein-viewer is used to help locate the veins.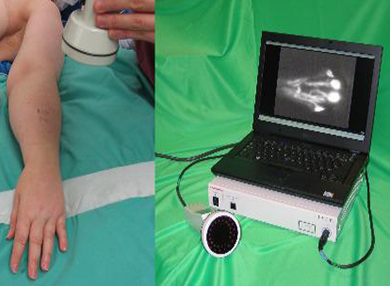
A technique known as indocyanine green (ICG) fluorescence lymphography is used in the clinic to determine suitability for LVA surgery. A green dye (ICG) is injected into the limb and a special scanner is used to map the lymphatic vessels and to see how well they are working. ICG is also used before surgery to help the surgeon determine where the connections will be made, and during surgery to check whether the connections made between the lymph vessels and the veins are working properly.
Internationally, ICG-assisted LVA surgery is rapidly becoming the surgical treatment of choice for early stages of limb lymphoedema. LVA was introduced to Macquarie University Hospital in August 2016. The operation takes from 3–5 hours and is performed by our surgeons who are highly trained in super-microsurgery.
Complications from LVA are uncommon, as the procedure is performed just below the surface of the skin and there is very little potential for damage. However, in rare cases the following complications may occur:
- problems with infection and wound healing
- complications related to general anesthesia
- allergic reaction to the ICG dye.
As a potential patient, you will be assessed at the MQ Health Lymphoedema Surgical Assessment Clinic by our multidisciplinary team, including plastic surgeon Dr Quan Ngo. Assessments will include a comprehensive clinical examination and standard tests, as well as imaging techniques such as lymphoscintigraphy, magnetic resonance imaging (MRI) and ICG lymphography. These tests will help us to determine your stage and extent of lymphoedema and your eligibility for LVA.
Criteria for selection
To be eligible for LVA, you must have:
- early-stage lymphoedema with some functioning lymphatic channels
- minimal skin and tissue changes (such as thickening or hardness)
- evidence of some movement of lymph fluid.
You will not be eligible for LVA if you have:
- a known allergy to iodine, shell fish or ICG dye
- recent infection (“cellulitis”) or inflammation of the skin in the affected limb
- undergone skin cancer treatment in the region of the affected limb
- had treatment for cancer within the last six months, including surgery, radiotherapy or chemotherapy
- conditions affecting your veins such as deep vein thrombosis or severe varicose veins involving the affected limb
- mainly fat deposition and irreversible changes in the soft tissue (best seen using an MRI)
- no functioning lymph vessels.
Compression garment
You will be fitted with a compression garment immediately after surgery and we will give you specific advice about your garment use when you are discharged.
Limb care
Limb elevation is recommended for the first 24 hours after surgery and we encourage you to do regular hand or foot circulation exercises. You can resume normal activities three to four days after surgery, and lifting, driving and light exercise after two weeks. You should avoid direct pressure on the surgical site and high-intensity use of your arm or leg (e.g. jogging, cycling, aerobic exercises, pump classes) for at least one month.
Hospital stay
LVA is usually a day surgery and you can usually go home on the same day or the next.
Infection prevention
It is important to keep the wound sites dry for three days to encourage healing. We also recommend that you use waterproof bandages when taking a shower. We will prescribe antibiotics and pain relief as required.
Prevention of deep vein thrombosis
If you have a predisposition for deep vein thrombosis, we will give you preventative medication.
You will be reviewed by the multidisciplinary team at MQ Health Lymphoedema Surgical Assessment Clinic on an ongoing basis at 1, 3, 6, 12, 18 and 24 months after your surgery. We will give you a full, clinical assessment at these visits. You will need a repeat ICG at 6 and 24 months.
You are also encouraged to continue with conservative lymphoedema treatment after your surgery as recommended by the lymphoedema therapist. This will include compression, massage, exercise and skin care. Your treatment regimen may be modified later based on your post-operative assessment.
To find out more about what the surgery involves, please contact our LVA team on 02 9812 2950.